Calls are an important part of a patient’s journey, and call detail records reporting and analytics can help optimize patient experience and improve outcomes after discharge from care.
Patients want clear communication. They do not want to wait endlessly on hold to get answers to important questions about their health. Hospitals also want to improve communication because it improves outcomes. Post-discharge calls have been shown to reduce readmission rates and can improve patient personal accountability and understanding of the importance of follow-up care.
Medicare Readmission Rate Penalties Cost Hospitals Millions
The Center for Medicare and Medicaid Services (CMS) recognizes the power of post-discharge communication, too. So much so, that they penalize hospitals over half a billion dollars each year for high readmission rates.
The CMS Hospital Readmission Reduction Program (HRRP) is a Medicare value-based purchasing program that began in 2012 that reduces payments to hospitals with excessive readmissions. Under HRRP, CMS encourages hospitals to avoid these costly financial penalties by better engaging patients and caregivers in post-discharge planning through improved communication and care coordination.
One recent study about readmission rates identified issues that contribute to high readmission including:
- Inability to reach providers or obtain a timely appointment
- Failed handoffs, due to abandoned calls and other communications problems
- Challenges with existing call-back programs such as large call volumes and inadequate staffing
In 2022, CMS penalized 2,499 hospitals a total of $521 million for having unacceptable readmission rates, with 39 hospitals receiving the maximum three percent reduction in payment. Since 2018, the annual fines have averaged over $200,000 per hospital.
Call Visibility Helps Improve Employee Productivity
Staffing shortages and cost increases, however, continue to push hospitals into the red and make goals of improving patient care and reducing costly readmissions difficult to attain. One effective way to help address this challenge is through improved patient call visibility.
Patient calls are being handled by different departments, offices, clinics, or specialists – not just through a hospital’s contact center – so it is essential for healthcare organizations to know their patients’ complete journey. Then, they can better understand hold time, and abandoned calls, and derive actionable information from this calling data to improve patient follow-up calls.
Studies show that well-managed patient follow-up call practices can reduce readmissions by 50%. Here are three ways healthcare organizations can gain complete patient calling visibility, increase patient satisfaction, and reduce readmissions and the risk of costly penalties:
Reduce Hold Times and Abandoned Calls with Hunt Group and Queue Visibility
One of the most common complaints from patients is long hold times and abandoned calls. This can leave patients feeling frustrated and dissatisfied with their experience, and disengaged from their care, increasing the possibility of readmission. To address this issue, healthcare organizations can implement call analytics solutions that provide real-time visibility into call queues and hunt groups. This can help identify bottlenecks and inefficiencies in call handling, allowing organizations to make data-driven decisions to improve call routing and reduce hold times.
Take, for example, a healthcare organization that receives complaints and patient surveys mentioning hold times that exceed 60 minutes. Unsurprisingly, many of these patients would be unable or unwilling to wait so long for a response, resulting in patients abandoning calls and not following their post-discharge care plan.
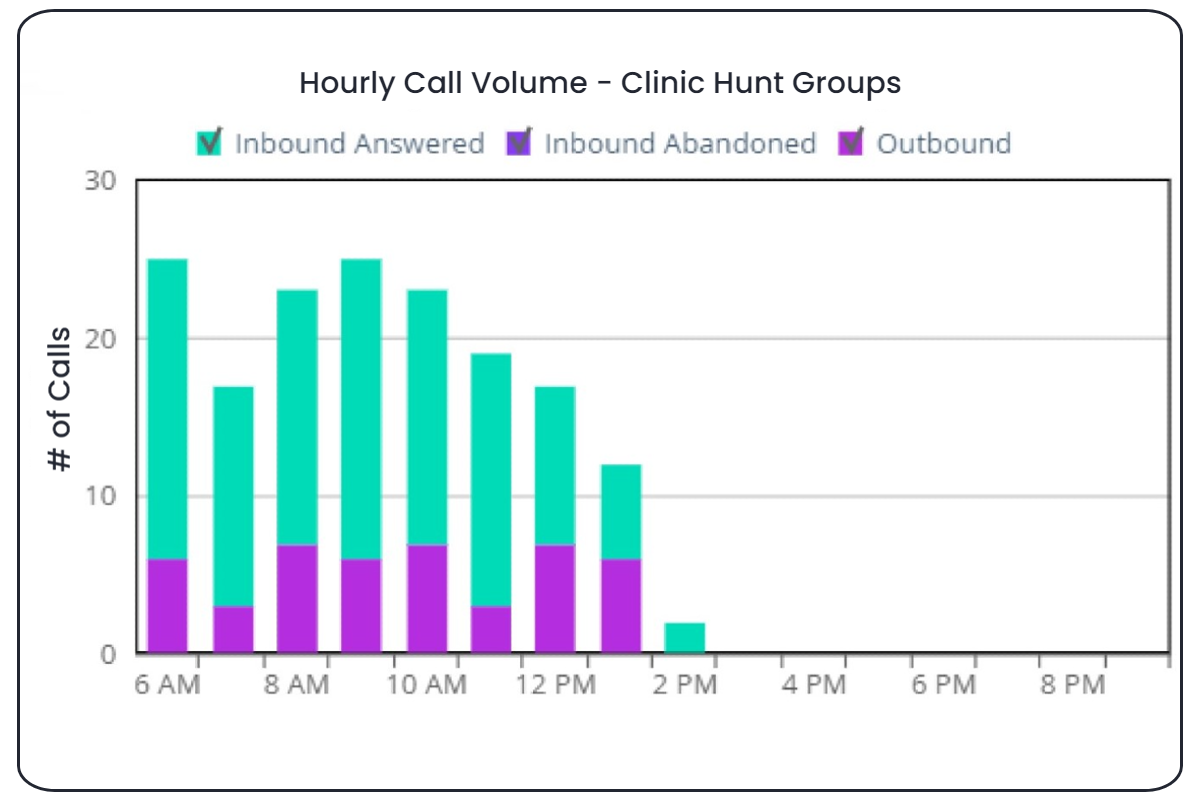
With enhanced queue analytics the hospital can see the problem before it escalates into horrible patient experience territory (like a 60-minute hold time), identify its root cause, and take corrective actions. Call queue analytics can identify low-performing call agents, and provide critical call performance data such as the total number of calls, calls handled, calls abandoned, call queue times, and drill-downs to secure hour of day details for each call. With this information, hospitals have a clearer view of patient communication so they can ensure that abandoned calls, excessively long hold times, and other poor patient experiences are minimized.
Use Cradle-to-Grave Call Analytics for Greater Visibility
Another way hospitals can improve their visibility into patient calling experience is through cradle-to-grave call analytics. This type of analytics allows healthcare providers to track calls from the moment they enter the system until they are resolved, providing a complete view of the patient experience. Cradle-to-grave is especially useful for identifying excessive or unnecessary call transfers and redirects.
By analyzing this data, healthcare providers can identify areas for improvement, such as call handling times, call routing, and communication with patients. This can help organizations make data-driven decisions to improve patient satisfaction and create a more positive patient experience. With cradle-to-grave, hospitals can study call flow to identify problems, excessive steps or conditions that result in excessive calls to voicemail or abandonment of calls.
For example, cradle-to-grave can provide better insight into employee productivity through extension-specific reports, Call Detail Record search, and redirection reports. This improved visibility is not only essential for seeing the entire patient calling journey, but also is essential for call handling compliance and guideline purposes, such as those contained in HRRP. With visibility into the complete cradle-to-grave calling experience, hospitals can also perform ad-hoc searches for related call segments by a variety of constraints, including Caller ID, involved extension numbers, number of related call legs, and more.
Gain Insights Easily and Quickly
Lastly, healthcare organizations can help improve patient experience and reduce readmission rates by using a solution that provides self-service reports optimized for line of business, not just IT. Healthcare providers can eliminate the need for extra IT resources or excessive delay in viewing calling metrics that are crucial for understanding the patient experience. Hunt Groups supervisors and patient experience staff require quick visibility into call progression to respond to caller complaints and as a tool for training and coaching employee performance.
A solution optimized for line of business can also provide access to popular pre-designed reports and handy drill-down to related call segments, or real-time hunt group or queue status. With access to these insights and more, organizations can more easily execute organization-wide initiatives for improving answer times, ensuring optimal staffing levels, and delivering the kind of patient experiences that encourage continued care and can reduce costs.
Caller experience is one area where hospitals can make impactful improvements in providing care, but staffing pressures and other issues can complicate monitoring and executing successful post-discharge call programs. The right call detail records analytics solution can not only help save hundreds of thousands to millions of dollars, it can also help improve patient care. Learn more about the many ways enhanced CDR analytics and reporting, such as ISI’s Premium Queue Analytics, helps hospitals better communicate with patients to optimize their care.

